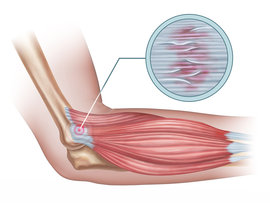
Tennis elbow, which is also known as lateral epicondylitis/epicondylalgia, is a painful condition that develops when the muscles and tendons that extend from the forearm to the outer portion of the elbow, called the lateral epicondyle, become injured or overworked.
This type of injury occurs commonly in tennis players as a result of repeatedly swinging the arm, and rapidly flexing and extending the wrist and elbow, all while gripping the racquet and forcefully contacting the ball, but anyone who moves the wrists, arms, and elbows in a repetitive motion can experience tennis elbow.
 In addition to tennis players, golfers, baseball players, factory workers, weight lifters, professional cleaners, bowlers, gardeners, and mechanics have an increased risk of developing this condition. The incidence of tennis elbow also tends to be higher in men than women. Tendon wear and tear or inflammation most often occurs due to poor technique, or training errors such as doing too much, too fast, for too long. For example, think of tennis players who live in colder climates. When spring arrives and the outdoor courts open, tennis enthusiasts often go full swing into play - without taking into consideration that they may not have kept up their tennis specific conditioning throughout the winter months. Their enthusiasm out paces their tissue response to load, leading to breakdown and pain.
In addition to tennis players, golfers, baseball players, factory workers, weight lifters, professional cleaners, bowlers, gardeners, and mechanics have an increased risk of developing this condition. The incidence of tennis elbow also tends to be higher in men than women. Tendon wear and tear or inflammation most often occurs due to poor technique, or training errors such as doing too much, too fast, for too long. For example, think of tennis players who live in colder climates. When spring arrives and the outdoor courts open, tennis enthusiasts often go full swing into play - without taking into consideration that they may not have kept up their tennis specific conditioning throughout the winter months. Their enthusiasm out paces their tissue response to load, leading to breakdown and pain.
Symptoms typically arise in an individual’s dominant arm and may include, but are not limited to the following:
- Burning or pain in the elbow region that gradually intensifies
- Pain that gets worse when an object is lifted or squeezed
- Experiencing intense pain or noticing a weak grip while grabbing objects
- Pain that worsens while moving the wrist (e.g., brushing the teeth, opening doors or jars)
Initially minor to moderate symptoms can typically be addressed by trying to find ways to rest the elbow in order to prevent further irritation. This means avoiding the aggravating activities when able but staying active and regularly moving and using the affected arm. Physical therapy is recommended to properly manage tennis elbow to fully explore why it occurred in the first place and what work or sport activities can be modified or corrected to allow the tissue to heal and withstand all your daily loads. A physical therapist can help individuals safely maintain strength and mobility in the elbow by demonstrating stretching exercises and strengthening techniques that support the body’s natural healing processes. Consult your primary care provider or pharmacist to see if a topical or an oral anti-inflammatory is indicated to help alleviate the initial pain. Keep in mind however, that many people with tendon overuse do not have active inflammation and the best way to reduce the pain is to exercise. A key form of exercise that helps target pain, while increasing muscle strength, is eccentric exercise.
For eccentric exercise, the key feature is controlling the load while the muscle lengthens - like doing a bicep curl and slowly lowering the weight, not letting it quickly drop back down. For a targeted tennis elbow eccentric exercise, you will initially need 1-3lbs (0.5-1.5 kg) of weight like a full water bottle, a light dumbbell, or even a canned product for gentle lifting. Your %physiotherapist’s% will have you sit with your forearm supported but wrist and hand free, such as sitting in a chair that has an armrest, or resting your forearm on a table with the hand dangling over the edge. Hold the item in your hand with the palm facing down to the floor, lift the wrist and hand until the wrist bends back and then return to the resting position with steady slow control. The exercise is repeated about 10-20 times (or to muscle fatigue) for 2-3 sets and should be performed 1-2 times a day.
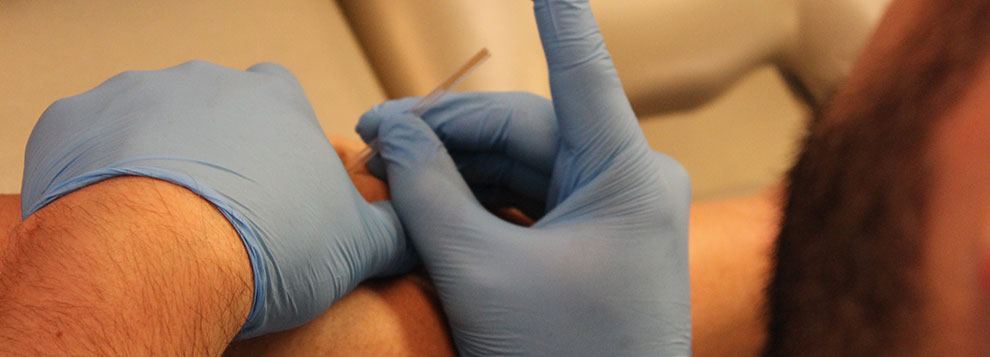
In addition to demonstrating these types of techniques, a physical therapist may recommend wearing an elbow brace as it provides extra support for the inflamed tendons and muscles. If necessary the physical therapy regimen may also involve a combination of tissue management approaches such as massage, shock wave therapy, or muscle stimulation techniques to enhance mobility and shorten recovery time. Clinical studies show that the majority of individuals with tennis elbow who work closely with a physical therapist can fully recover without the need for more invasive treatments.
The proper management of tennis elbow is one of the keys to experiencing long-term relief, but a highly skilled physical therapist can also help you identify specific activities or parts of your daily routine that may have contributed to the injury, thereby helping prevent further problems in the future. The physical therapists at Iron City Physical Therapy can design a program just for you that will help restore the mobility and function of your elbow.
References
1. Shiri R, Viikari-Juntura E, Varonen H, Heliövaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol. 2006; 164(11):1065-74. 2. Weber C, Thai V, Neuheuser K, Groover K, Christ O. Efficacy of physical therapy for the treatment of lateral epicondylitis: a meta-analysis. BMC Musculoskelet Disord. 2015;16(1):223. 3. Peterson M, Butler S, Eriksson M, Svärdsudd K. A randomized controlled trial of eccentric vs. concentric graded exercise in chronic tennis elbow (lateral elbow tendinopathy). Clin Rehabil. 2014;28(9):862-72. 4. Croisier JL, Foidart-Dessalle M, Tinant F, Crielaard JM, Forthomme B. An isokinetic eccentric programme for the management of chronic lateral epicondylar tendinopathy. Br J Sports Med. 2007;41(4):269-75. 5. Ng GY, Chan HL. The immediate effects of tension of counterforce forearm brace on neuromuscular performance of wrist extensor muscles in subjects with lateral humeral epicondylosis. J Orthop Sports Phys Ther. 2004;34(2):72-8. 6. Gündüz R, Malas FÜ, Borman P, Kocaoğlu S, Özçakar L. Physical therapy, corticosteroid injection, and extracorporeal shock wave treatment in lateral epicondylitis. Clinical and ultrasonographical comparison. Clin Rheumatol. 2012;31(5):807-12.